Postnatal Care 3: 4-8 weeks following delivery
During the first 4 weeks after delivery it is a crucial time for rest and recovery, wound support, and early muscle rehabilitation. By 4-6 weeks you’re probably starting to wonder when you can start to increase your physical activity and return to exercise? So we wanted to shed some light and give some advice on this topic, along with other common questions or concerns related to this postpartum period.
Postnatal Pelvic floor assessment and return to exercise:
We advise all women to see a women’s health physio after birth regardless of delivery (vaginal or C-section), we recommend any time after 6 weeks, mainly because of the healing that occurs in that first 6 weeks. You might be wondering why you would have to see a physio when you are already going to see your GP or OBGYN at this 6-week mark anyway? In reality, the vast majority of what goes on in your GP or OBGYN appointment is actually centred around the health and well being of your newborn baby. In general the pelvic floor muscles are not assessed and there is very little discussion about a plan for gradual, individualised return to exercise.
And that’s to be expected, these musculoskeletal assessments and exercise prescriptions are not the domain of obstetricians, midwives and GP’s. Their specialities are delivering babies and ensuring that mother and baby are medically well. These are instead the domain of Women’s health physios.
So what is to be expected at the check up?
Internal pelvic floor assessment checking for pelvic floor muscle tone, strength, endurance, coordination and any fascial damage or pelvic organ prolapse.
Abdominal muscle separation check - continue to wear your compression garments e.g. tubigrip or SRC shorts until this assessment to ensure you have the support for your abdominals and back (see last post for more info on this topic).
Musculoskeletal assessment for back pain, pelvic pain, wrist pain, postural dysfunction - feeding, picking up and holding bub are all positions and activities that can cause cranky bodies so we provide stretches and advice on how to reduce your discomfort.
Bladder and bowel function screening.
Following the assessment, we can then create an individualised rehabilitation and safe return to exercise plan.
Generally speaking however, at this point it is important to introduce some gentle functional exercise:
You can start to slowly increase your walks being sure to listen to your body. You shouldn’t feel any downward pressure through the vagina or have any leakage.
If comfortable, you can begin exercising on a stationary bike, as this doesn’t put too much pressure through the pelvic floor, just avoid standing up on the pedals!
You may begin some swimming or gentle water-based exercises (once bleeding has stopped and wounds have healed!).
Abdominal bracing and specific exercises - if you have abdominal muscle separation, it is important to check with your women’s health physio to ensure you are using your abdominal muscles correctly.
Low impact post-natal class with an instructor who specializes in women’s health.
Ensure you stretch regularly to reverse prolonged activities such as feeding - check in on our social media this week for examples of great stretches.
Remember that even though you may feel ok, there are still hormones affecting the laxity of your ligaments which can affect the stability throughout your whole body, so always listen to your body and if what you are doing doesn’t feel ok, wait until you can get some advice from your health care practitioner.
Continuing wound care (perineal and c-section scar):
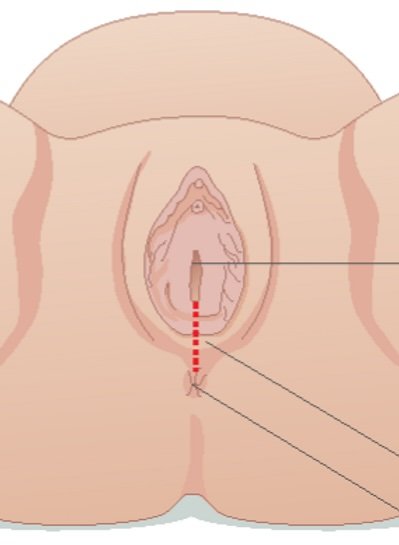
The perineum is the firm piece of skin at the base of the vagina, between the vagina and bowel. The tissue is prone to tears during childbirth, and can often have stitches and a subsequent scar. After you have been advised by your GP or OBGYN at your 6 week check that the wound is healed and clear of any infection, it is a good idea to begin gentle scar massage to help it heal by mobilising and increasing blood flow to the area.
Signs of a tight perineal scar:
- Pain with sex or use of tampon.
- Discomfort when wiping after going to the toilet.
C-section scars can often be a source of anxiety and worry for a lot of women. For this reason, a lot of women are reluctant to touch the scar. But can suffer from a lot of pain.
Signs of a tight scar:
- Firm pieces of skin that are uncomfortable to touch.
- Pulling or tugging when trying to stand upright.
- Pain or discomfort at the scar site.
If you are noticing any signs of a tight scar it is recommended that you see your healthcare practitioner to ensure there are no signs of infection or concerns about the scar, and to get specific advice on how to perform a massage and where to target.